Needleless Connectors and Bacteremia: Is There a
Relationship?By Marilyn Hanchett, RN, PhD
November 1, 2005
Abstract
http://www.infectioncontroltoday.com/articles/2005/11/needleless-connectors-and-bacteremia-is-there-a-r.aspx
Needleless connectors, used today as integral
components of an infusion system, evolved in
response to demands for enhanced healthcare worker
safety and as part of the continuing development of
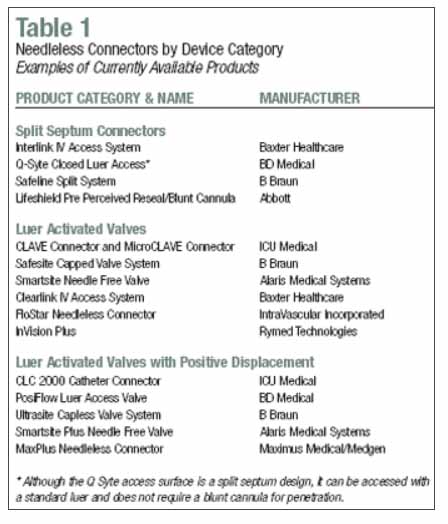
infusion technology. At this time, there are three
design categories among needleless connectors: split
septum connectors, luer activated valves, and luer
valves with positive displacement. Numerous branded
products are available within each category.
Although needleless connectors offer enhanced safety
features, there have been recurrent concerns about
an increased risk of bacteremia associated with
their use. This article reviews the development of
these devices, examines the available evidence base,
identifies unresolved issues, and suggests
strategies to facilitate optimum use of needleless
connectors within infusion systems.
Introduction
During the past two years there has been
increasing concern expressed by infection control
practitioners, infusion specialists, and
epidemiologists that the use of needleless
connectors, either generally or specifically
according to design category or brand, is directly
responsible for increased bacteremia inpatients
receiving intravenous therapy.
Bacteremia associated with infusion therapies is
known to increase morbidity, prolong inpatient
hospitalizations, and significantly increase the
economic impact of care.1 The incidence
of catheter-related bloodstream infections is
disturbingly high, especially among central
catheters, and the mortality risk has been reported
as high as 30 percent in ICUs.2 Since
intravenous therapy is among the most widely used
invasive procedures in all healthcare settings, the
risk of complications is often also high. If any
part of an intravenous system increases patient
risks, then the clinician must be aware of it and be
prepared to respond accordingly.
The Evolution of Needleless Connectors
First Generation Products
Prior to the 1980s, intermittent access to
an intravenous system was accomplished by inserting
a beveled, hollow bore needle into a latex cap
positioned either along the administration set or at
its termination. The needle was often secured with
tape and was prone to disconnection. Emerging
technology soon combined with engineering controls
required under the Occupational Safety and Health
Administration (OSHA) Boodborne Pathogens Standard
to produce a new generation of connectors.
This first generation of devices featured a split
septum that could be repeatedly accessed with a
blunt cannula. These connectors were designed to
accommodate the need for intermittent access to the
intravenous system while simultaneously eliminating
the use of needles. The split septum connectors were
used in combination with other emerging technology,
including safety catheters that typically offered
recessed or retractable needles. Although this new
technology was neither immediately nor universally
adopted and the costs associated with its use often
posed a barrier to implementation, these first
generation safety products were successful in
reducing the exposure incidents reported by
healthcare workers.3 However, the first
generation split-septum products did not address the
problem of catheter occlusion. Split-septum
connectors created negative pressure when the blunt
cannula was withdrawn. Any negative pressure at the
time of disconnection can jeopardize device patency
by allowing retrograde flow into the lumen of the
catheter.
Second Generation Products
During the 1980s, technology continued to
evolve. The second generation of needleless
connectors replaced the split-septum design with an
anti-reflux valve activated by the use of a
malefemale luer configuration. The process of
joining the luer components created a locking action
that exceeded the stability of the connection
possible with the splitseptum product. Since female
and male luer mechanisms were already a
well-established concept within medical device
design, the integration of a luer into a connector
was easily understood and accepted by clinicians.
Like the first generation of connectors, the luer
devices permitted intermittent access and eliminated
the use of needles. However, its unique design was
compatible with the use of most syringes and the
need for a blunt cannula was eliminated. In
addition, the ant-reflux design of the luer
activated valve helped neutralize any negative
pressure occurring when the syringe (or other luer
device) was disconnected from the needleless
connector. And when used according to manufacturer
guidelines, these products did not demonstrate an
increased safety risk.
Unfortunately, the luer compatible design has
been demonstrated to pose other, non-infectious
safety risks to patients. The serious incidents that
have been reported have all involved incorrect
product use. For example, in 1996 and 2002 the
Institute for Safe Medicine Practices cautioned the
healthcare industry about the potential to connect a
syringe containing oral medication to an intravenous
system by attaching it to a needleless valve.4
In 2003, the Food and Drug Administration (FDA)
issued a safety alert following a patient death when
oxygen was accidentally connected to a needleless
luer device.5 However, during these years
intravenous systems were also evolving. Implanted
infusion ports were introduced for patients
requiring long-term therapies.
Tunneled central catheters became a viable option
for patients no longer candidates for peripheral
infusions. Peripherally inserted central catheters
(PICCs) offered a safer alternative when therapy was
expected to continue for more than several days.
Third Generation Products
With more advanced catheter design and the
clinical demand for extended catheter dwell times,
the need to maintain patency became a growing
clinical concern. Replacement of clotted catheters
was expensive and traumatic for the patient. A
clotted lumen can also increase the risk of
infection. A number of solutions emerged to address
this need, including the development of a valved
catheter, the use of fibrinoloytics for catheter
clearance, and the introduction of a positive
displacement connector.
The third generation of connectors combined the
existing lueractivated valve concept with a
displacement action. This action expels a small
amount of the solution used to flush the catheter
when the syringe used for flushing is disconnected
from the leur. The displacement is a passive feature
and occurs automatically. Once this action has
occurred, the remaining solution (usually heparin or
saline) is retained within the catheter and no
further positive pressure exists. The positive
pressure luer connector is designed to reduce
retrograde flow into the catheter more effectively
that either split-septum or standard luer
connectors.
However, although the third generation of
connectors offered advantages over previous designs,
they cannot prevent occlusion completely or under
all circumstances. Nonetheless, positive
displacement connectors are now widely used to help
reduce complications in central catheters. Today,
examples of split-septum, luer-activated and
positive displacement luer connectors are
commercially available and commonly used in
intravenous systems (see Table 1).
Emerging Infection Concerns
The gradual introduction of and product
diversification within needleless connectors was
accompanied in the 1990s by concerns regarding their
infection risks. Studies published during this time
period revealed a number of issues that could
potentially lead to increased infections. For
example, needleless connectors were not always used
according to manufacturer guidelines. Infection
risks increased when connectors were changed less
frequently than specified in protocols.6-8
An increased infection risk was also linked to
specific infusates such as TPN or other independent
risk factors such as use of multilumen catheter or
recent BMT.9-10
Although a variety of needleless connectors were
investigated, no individual products were
conclusively associated with either increased risk
or national outbreaks. While initial concerns
focused on device failure, a better understanding of
device use in conjunction with enhanced product
design, helped allay clinician fears and allow
needleless connectors to remain an integral safety
component of most, if not all, intravenous systems.
In fact in 2002 the HICPAC IV Guideline stated that
“when devices are used according to manufacturer’
recommendations, they do not substantially affect
the incidence of CRBSI.”11
A Limited Base of Evidence
Since the 1990s, concerns have lingered about the
relationship of needleless connectors to bacteremia.
Infection control experts have remained alert to the
serious complications that can potentially be
associated with these seemingly innocuous devices.
But the need for better device-related science
remains an elusive goal.
A review of the literature indicates that the
studies of the 1990s have not been significantly
expanded by subsequent experimental research. In
fact, although millions of needleless connectors are
used in patient care, the scientific evidence upon
which to base their use remains limited. Current
studies vary widely in their scope, design, and
scientific rigor.
For example, from 1999 to 2004, three new studies
attempted to examine the efficacy of positive
pressure in maintaining the patency of central
venous catheters. These prospective studies show
that positive displacement of fluid within central
catheters is more effective than negative pressure
(or displacement) in preventing occlusions. However,
these studies also show that the positive
displacement action accomplished with valve
technology cannot eliminate the problem of occlusion
in all central venous catheters.12-14
Recent published reports have investigated the
issue of infection. Two studies, using different
products, have reported a reduced potential for
microbial contamination when traditional caps were
replaced with a needle-free, luer valve that was
been appropriately disinfected prior to use.15-16
As risks associated with needleless connectors
have become an international infection control
concern, published reports are now available in
non-U.S. based clinical journals. For example, an
evaluative study conducted in Britain reported
inconsistency of use and routine care of all
connectors used with central catheters prior to
staff education and standard implementation of a
luer valve.17 A randomized controlled
trial conducted in Spain among intensive care
patients requiring central venous catheters found a
significant reduction in bacteremia when a
needleless connector was used in place of a
three-way stopcock.18
In addition to the studies published in
scientific, peer-reviewed journals there are also a
number of product evaluation studies or reports that
have appeared in clinical practice journals, on Web
sites, and in trade publications. These articles
generally describe an institution’s experience in
using a needleless connector or after changing
brands. This level of evidence is typically
presented either as a quasi-experimental study or as
descriptive research and lacks the scientific rigor
and control used in the experimental designs. Their
lack of control is especially problematic when
attempting to infer causation and/or generalize the
findings to other practice settings.
Understanding the Current Controversy
Similar to the experiences of a decade ago,
reports of bacteremia have resurfaced. The implied
cause of these new or increased infection rates
appears to be the use of needleless connectors.
Concern about the use of needleless connectors has
been expressed in presentations, posters, and/or
abstracts presented at annual meetings such as the
Society of Healthcare Epidemiologists of America
(SHEA), the Association for Professionals in
Infection Control and Epidemiology (APIC), and other
professional organizations since 2004.
Simultaneously, some manufacturers have attempted to
leverage infection concerns to better position their
individual brands. For clinicians struggling to
understand the issue, the result is often a
confusing jumble of genuine, albeit unanswered,
device concerns with product marketing claims, data
from bench studies, expert speculation, and
over-generalization of findings from institutional
reports.
The dilemma remains, as it did a decade ago, the
same for all who currently attempt to analyze the
infectious risk potential of these devices. There is
simply not enough scientifically rigorous evidence
upon which to make a conclusion. Although there have
been sporadic reports of increased infections, there
is insufficient evidence to indicate a trend that
can be reliably associated with a specific type of
connector or any particular product.
Potential Risk Factors Requiring Further
Investigation
In order to fully understand the risk potential
of any type or brand of needleless connector,
several important factors need to be clarified.
1. User Error or Device Failure?
Most published reports have not measured the
potential for user error. Any break in aseptic
technique when using a needleless connector sets the
stage for potential infection. At this time, the
lack of information related to user error with
needleless connectors is a significant barrier in
analyzing the underlying cause of actual or presumed
increases in bactermia. Although the devices are
mechanically simple and their use intuitive, user
errors can still occur. For example, clinicians may
not disinfect the surface of the connector before
accessing the intravenous system. Connectors may not
be flushed completely after use or may not be
changed according to established protocols. Luer
valves may not fully rebound upon disconnection.
Split-septum connectors may be damaged by incorrect
access with a needle or an incorrectly placed needle
rather than a blunt cannula. Extension sets,
attached to connectors and intended for intermittent
IV access, may not be clamped as required by the
manufacturer.
In any study that attempts to identify causation,
it is essential that all reasonable contributing
variables be identified and controlled. Without this
essential step, it is easy to draw the wrong
conclusion. Allegations of device failure are often
the initial and presumptive cause attributed to
sudden increases in bloodstream infections. While
concern over device failure is a possibility that
must always be considered, it cannot be presumed to
the primary cause when insufficient evidence exists
to support the claim. At the same time, designing a
clinical study that can achieve the necessary level
of control is very challenging and can be cost
prohibitive for the sponsoring institution. This is
particularly problematic when studying needleless
connectors since both the number of potential users
and opportunities for intentional or accidental
misuse is high in all practice settings where
infusion therapies are administered.
The potential impact of incorrect use cannot be
ignored, especially since the study by Cookson et
al. reported that only 60 percent to 70 percent of
nurses maintained needleless connectors correctly.6
While procedural compliance by clinicians performing
infusion therapy has not been thoroughly studied,
other aspects of infection control have been.
Perhaps the best-known focuses on hand washing
where, no matter how frequent or extensive the
education provided, clinician compliance rarely
exceeds 40 percent.22 If compliance with
the use of needleless connectors is similar to
compliance with handwashing, user error could emerge
as the most important contributing factor in
device-related infections. At this time, however, it
remains an unknown variable.
2. Device Design In spite of marketing claims to
the contrary, the superiority of one type of design
for needleless connectors has not been proven. In
fact, the impact of residual volumes, dead spaces,
and flow rates on infection risk has not been
extensively analyzed. Manufacturers will inoculate
the access surface and/or the fluid pathway of their
device with bacteria to test, under strict
laboratory conditions, the efficacy of surface
decontamination with an approved disinfectant as
well as the possibility of bacterial growth and
transfer along the fluid pathway. Such testing is
usually limited to seven or eight consecutive days.
Longer-term outcomes, especially in less rigidly
controlled environments, have not been discussed in
the literature.
Part of the current controversy focuses on
determining whether split septum or luer-activated
valve technology represents the safest approach in
preventing catheter-related bloodstream infections.
Until more evidence exists regarding the impact of
mechanical design aspects on infection risk, none of
the three currently available categories of
needleless connectors can claim superiority.
3. The Impact of Biofilm Microbial biofilm is the
accumulation of polymers excreted by bacterial cells
adhering to a device surface. The accumulation of
biofilm on medical devices, including intravenous
catheters, cannot be prevented and creates clinical
management challenges for long-term, indwelling
devices. Biofilm accumulates rapidly on central
venous catheters and once in place, is difficult to
eradicate. Biofilm-related infections often require
removal of the device.19
There has been minimal investigation on the role
that biofilm may play in the needleless connector
controversy. A study published in 2001 examined
needleless connectors used at a bone marrow
transplant center. The results of this analysis
showed that 63 percent of the 24 needleless
connectors tested contained biofilms comprised
predominantly of coagulase-negative staphylococci.20-21
These results suggest additional questions. If
biofilm has been detected on central venous
catheters is less than 72 hours after placement, is
development within needleless connectors equally as
rapid? Is the accumulation of biofilm facilitated by
mechanical design aspects of these devices? Does
biofilm demonstrate an affinity for split-septum
products, luer-activated valves, or is there no
difference? Answers to these and many other
questions will remain unanswered until more research
is done.
Taking Action When Evidence is Lacking
The lack of reliable evidence, although highly
problematic, is not an insurmountable obstacle for
ICPs urgently seeking to prevent bacteremia in
patients receiving infusion therapies. Awareness of
a limited evidence base helps direct decisions and
actions along lines of the best available data and
objective reasoning. The following list summarizes
steps that infection control practitioners can take
now.
- Use interdisciplinary collaboration to
verify that surveillance systems and collection
of epidemiological data for intravenous
procedures are adequate. Although
device-specific surveillance often focuses on
critically ill patients, risks may also be high
among those who are less acutely ill but require
long-term catheters and therapies. Collaboration
is essential in identifying these patient groups
and mobilizing the resources to conduct the
necessary data collection and analysis.
- Critically examine the impact of intravenous
education and training in your institution.
Although infusion therapy is among the most
commonly performed invasive procedures, most
clinicians have received very little formal
education about it. While manufacturers can
provide excellent in-service programs and
training materials, it is the responsibility of
the institution to make sure that procedural
compliance and infection control standards are
maintained, reinforced and reviewed as often as
necessary to meet patient care goals.
- Carefully analyze all product literature and
studies. Understand the scope of published
studies and whether their design, methods,
findings, and conclusions meet the standards of
scientific evidence. Insist that claims of
product superiority be supported with reliable
information. Be an informed, skeptical, and
objective consumer when confronted with product
marketing.
- Remember that while intravenous therapy
systems and products are always changing and it
is important to keep current with new
technology, no product can replace sound
clinical judgment, critical decision-making, and
rigorous infection control practice.
- Look for new scientific evidence. Research
in the use of needleless connectors, and
especially the impact of biofilm, continues and
clinicians should expect that the current
evidence base with be expanded by future
studies.
- Involve your patients. This is especially
important in patients who require long-term or
chronic therapies. These individuals are often
experts in managing their catheters and supplies
that far exceed that of many healthcare
professionals; their feedback can be an
important addition to your regular sources of
information and evaluation.
Conclusion
Needleless connectors, initially designed to
reduce needlestick exposures among clinicians, have
contributed to a safer workplace and helped reduce
the injury risks associated with performing infusion
procedures. Whether or not needleless connectors
increase the risk of bacteremia or prevent catheter
occlusion is less certain.
Effectiveness of intraluminal fluid displacement
triggered by specific valved connectors is suggested
by current studies but has not been extensively
examined in the literature. At the same time, as
needleless connectors have been the alleged cause of
infection outbreaks, studies have failed to
conclusively demonstrate the link or identify any
product trends. Many products have been investigated
but none have shown greater or lesser risk for
potential infections. Many important variables in
the infection equation, including user error,
mechanical design, and the role of biofilm, remain
unknown.
Like all medical products, needleless connectors
present the clinicians with both advantages and
disadvantages. And like other products, they are
only as safe and reliable as the individuals using
them. Until conclusive evidence becomes available to
differentiate among existing products or as part of
a new generation of products, clinicians must
continue to include monitor needleless connectors,
evaluate device-related outcomes, and seek to better
understand the potential for user error within all
practice settings. ICT Marilyn Hanchett, RN, PhD,
is director of clinical affairs for IgG America.
References
1. Mermel LA. Prevention of intravascular
catheter-related infections. Annals of Internal
Med 2000; 132: 391-402.
2. Pittet D, Tarara D, Wenzel RP. Nosocomial
bloodstream infection in critically ill patients.
Excess length of stay, extra costs and attributable
mortality. JAMA 1994; 271: 1598-601.
3. Lawrence LW et al. The effectiveness of a
needleless intravenous connection system: an
assessment by injury rate and user satisfaction.
Infection Control Hosp Epidemiology 1997 March;
18 (3):175-82.
4. FDA Safety Alert. Subject: Clearlink System.
May 13, 2004. Food and Drug Administration,
Washington, D.C.
5. Medication Safety Alert, June 17, 2004:
Problems persist with lifethreatening tubing
misconnections. Institute for Safe Medication
Practices, Philadelphia, Pa.
6. Cookson ST, Ihrig M, O’Mara EM. Increased
bloodstream infection rates in surgical patients
associated with recommended use and care following
implementation of a needleless device. Infection
Control Hosp Epidemiology 1998; 19:23-7.
7. Do AN, Ray BJ, Banerjee SN et al. Bloodstream
infection associated with needleless device use and
the importance of infection control practices in the
home healthcare setting. Journal of Infect Dis
1999; 179: 442-41.
8. McDonald LC, Banerjee SN, Jarvis WR.
Line-associated bloodstream infections in pediatric
intensive care unit patients associated with a
needleless device and intermittent intravenous
therapy. Infect Control Hosp Epidemiology
1998; 19: 77-
9. Danzig LE, Short LJ, Collins K, Mahoney M.
Sepe S, Bland L, Jarvis WR. Bloodstream infections
associated with a needleless intravenous infusion
system in patients receiving home infusion therapy.
JAMA 1995 Jun 21: 273(23): 1862-4.
10. Tokars JI, Cookson ST, McArthur MA, Boyer CL,
McGeer AJ, Jarvis WR. Prospective evaluation of risk
factors for bloodstream infection in patients
receiving home infusion therapy. Annals Internal
Med. 1999 Sept 7; 131 (5): 340-7.
11. O’Grady NP, Alexander M, Dellinger P, et al.
Guidelines for the prevention of intravascular
catheter-related infections. Centers for Disease
Control and Prevention. MMWR Recomm Rep. 2002 Aug
9;51(RR - 10):1-29.
12. Hoffer EK, Borsa J, Santulli P et al.
Prospective randomized comparison of valved vs.
nonvalved peripherally inserted central vein
catheters. Am Journal Reontgenol. 1999: 173:
1393-98.
13. Hoffer EK, Bloch RD, Borsa J et al.
Peripherally inserted central catheters with distal
vs. proximal valves: prospective randomized trial.
Journal Vasc Interv Radiology 2001: 12:
1173-77.
14. Jacobs BR, Schilling S, Doellman D et al.
Central venous catheter occlusion: a prospective,
controlled trial examining the impact of a positive
pressure valve device. Journal Parenter Enteral
Nutrition 2004: 28: 113-8.
15. Bouza E, Munoz P, Lopen-Rodtrquex J et al. A
needleless closed device (CLAVE) protects from
intravascular catheter tip and hub colonization a
prospective randomized study. Journal Hosp
Infection 2003 Aug: 54(4(: 279-87.
16. Casey AL, Worthington T, Lambert PA et al. A
randomized, prospective clinical trial to assess the
potential infection risk associated with the
PosiFlow needleless connector. Journal Hosp
Infect. 2003 Aug: 54(4): 288-93.
17. Cheesman D. Intravenous care: the benefits of
closed system connectors. British Journal Nurs.
2001 Mat 8-21; 10(5): 287-95.
18. Yebenes JC, Vidaur L, Serra-Prat M et al.
Prevention of catheter-related bloodstream infection
in critically ill patients using a dsinfectable,
needle free connector: a randomized controlled
trial. Am Journal Infect Control 2004 Aug;
32(5): 291-5.
19. Ryder M. Catheter-related infections: it’s
all about biofilm. Topics in Advanced Practice
Nursing eJounral 2005; 5(3) 2005 Medscape.
20. Donlan RM, Murga R, Bell M, Toscano CM, Carr
JH, Novicki TJ, Zuckerman C, Corey LC, Miller JM.
Protocol for detection of biofilms on needleless
connectors-attached to central venous catheters.
Journal Clinical Microbiol. 2001 Feb;
39(2):750-3.
21. Biolfilms and device-associated infections.
Emerging Infect Dis. 2001 Mar-Apr;
7(2):277-81.
22. Kuzu N, Ozer F, Aydemir S, Yalcin AN, Zencir
M. Compliance with hand hygiene and glove use in a
university-affiliated hospital. Infection Control
Hosp Epidemiology 2005 Mar; 26(3): 312-5.
Click here to purchase reprints |